Epilepsy Facts & Treatments
You can’t swallow your tongue during a seizure. It's physically impossible.
You should NEVER force something into the mouth of someone having a seizure. Absolutely not! Forcing something into the mouth of someone having a seizure is a good way to chip teeth, cut gums, or even break someone's jaw. The correct first aid is simple. Just gently roll the person on one side, support their head, protect from injury, and make sure their breathing is okay.
DON'T restrain someone having a seizure. Most seizures end in seconds or a few minutes and will end on their own. You can protect the person from injury by following simple first-aid guidelines.
Epilepsy is NOT contagious. You simply can't catch epilepsy from another person.
Anyone can develop epilepsy. Seizures start for the first time in people over age 65 almost as often as it does in children. Seizures in the elderly are often the after effect of other health problems like stroke and heart disease.
Most people with epilepsy CAN DO the same things that people without epilepsy can do. However, some people with frequent seizures may not be able to work, drive, or may have problems in other parts of their life.
People with epilepsy CAN handle jobs with responsibility and stress. People with seizure disorders are found in all walks of life. They may work in business, government, the arts and all sorts of professions. If stress bothers their seizures, they may need to learn ways to manage stress at work. But everyone needs to learn how to cope with stress! There may be some types of jobs that people with epilepsy can’t do because of possible safety problems. Otherwise, having epilepsy should not affect the type of job or responsibility that a person has.
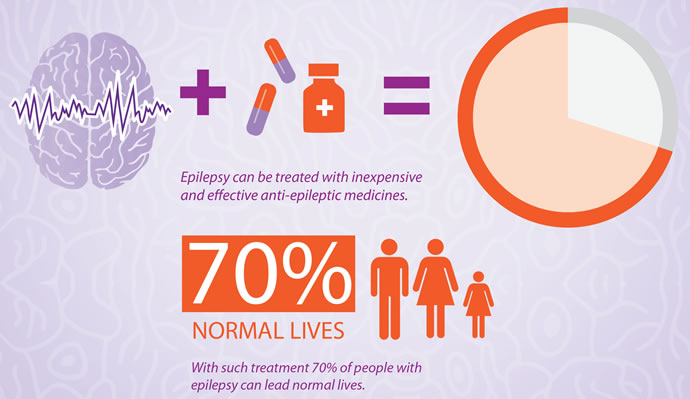
Even with today's medication, epilepsy CANNOT be cured. Epilepsy is a chronic medical problem that for many people can be successfully treated. Unfortunately, treatment doesn't work for everyone. AT LEAST 1 million people in the United States have uncontrolled epilepsy. There is still an urgent need for more research, better treatments and a cure.
You CAN die from epilepsy. While death in epilepsy doesn't happen frequently, epilepsy is a very serious condition and individuals do die from seizures. The most common cause of death is SUDEP or Sudden Unexpected Death in Epilepsy. While there is a lot we still don’t know about SUDEP, experts estimate that one out of every 1000 people with epilepsy die from SUDEP each year. People can also die from prolonged seizures (status epilepticus). About 22,000 to 42,000 deaths in the US each year occur from these seizure emergencies.
What happens in a seizure may look different from one person to another. However, seizures are usually stereotypic, which means the same things or behaviors tend to occur in a person each time they have a seizure. The seizure behavior may be inappropriate for the time and place, but it is unlikely to cause harm to anyone.
Epilepsy is NOT rare. There are more than twice as many people with epilepsy in the US as the number of people with cerebral palsy (500,000), muscular dystrophy (250,000), multiple sclerosis (350,000), and cystic fibrosis (30,000) combined. Epilepsy can occur as a single condition, or may be seen with other conditions affecting the brain, such as cerebral palsy, intellectual disability, autism, Alzheimer's, and traumatic brain injury.
People with epilepsy are usually not physically limited in what they can do. During and after a seizure, a person may have trouble moving or doing their usual activity. Some people may have trouble with physical abilities due to other neurological problems. Aside from these problems, a person who is not having a seizure is usually not limited in what they can do physically.
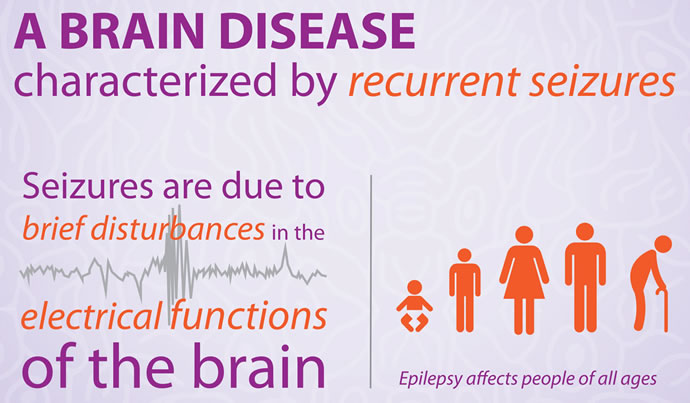
Epilepsy is a disorder in which nerve cell activity in the brain is disturbed, causing seizures.
FACTS
- It's Common
- 200,000 to 3 million US cases per year
- Can't be cured, but treatment may help
- Requires a medical diagnosis
- Lab tests or imaging often required
- Chronic: can last for years or be lifelong
- During a seizure, a person experiences abnormal behavior, symptoms, and sensations, sometimes including loss of consciousness. There are few symptoms between seizures.
- Epilepsy is usually treated by medications and in some cases by surgery, devices, or dietary changes.
SYMPTOMS
- Requires a medical diagnosis
- During a seizure, a person experiences abnormal behavior, symptoms, and sensations, sometimes including loss of consciousness. There are few symptoms between seizures.
- People may experience:
- Muscular: rhythmic muscle contractions or muscle spasms
- Cognitive: amnesia or mental confusion
- Sensory: aura or pins and needles
- Whole body: fainting or fatigue
- Psychological: depression or fear
- Also common: seizures, anxiety, headache, sleepiness, staring spells, or temporary paralysis after a seizure
Consult a doctor for medical advice
TREATMENTS
Can't Be Cured, But Treatment May Help
- Epilepsy is usually treated by medications and in some cases by surgery, devices, or dietary changes.
- Prescription
- Carbamazepine (Tegretol), Diazepam (Valium), Topiramate (Topamax), Lamotrigine (Lamictal), Oxcarbazepine (Trileptal), Midazolam by injection, Gabapentin (Neurontin), Levetiracetam by injection or by mouth (Keppra), Clonazepam (Klonopin), Phenobarbital, Primidone (Mysoline), Ethosuximide (Zarontin), Pregabalin (Lyrica), Felbamate (Felbatol), Phenytoin by mouth (Dilantin) or by injection, Valproic acid (Depakene)
- Specialists
- Neurologist: Treats nervous system disorders
- Primary care provider (PCP): Prevents, diagnoses, and treats diseases.
- Neurosurgeon: Specializes in nervous system disorders.
Source: World Brain Day 2015
What is a seizure?
To understand what a seizure is, you must first understand how the brain works. Your brain is comprised of thousands of neurons – cells that process and transmit information by interacting with each other. These interactions can be observed and assessed through an electroencephalogram (EEG).
In most brains, neuron interactions occur in a chaotic but balanced, orderly fashion with few disruptions. Occasionally, small disruptions (neuron misfires) may occur with little consequence. When multiple cells misfire at the same time – depending on the severity and location in the brain – it may cause muscle twitches and spasms. This is a seizure. A seizure is defined as a sudden, electrical discharge in the brain causing alterations in behavior, sensation, or consciousness.
The difference between “epilepsy” and “seizures” -
Many believe that having a seizure equates to having epilepsy. Although the two terms are often used simultaneously, a seizure (which is a single occurrence) is different than epilepsy (which is defined as two or more unprovoked seizures).
Seizures that appear to begin everywhere in the brain at once are classified as generalized seizures, while those beginning in one location of the brain are classified as partial seizures.
The three stages of a seizure:
Aura – The start of a partial seizure. If the aura is the only part an individual experiences, they’ve had a simple partial seizure. If the seizure spreads and affects consciousness, it is known as complex partial seizure. If the seizure spreads to the rest of the brain, it is classified as a generalized seizure.
Ictus – Meaning stroke or attack, ictus is another word for the physical seizure.
Postictal – Meaning after the attack, postictal refers to the aftereffects of the seizure, e.g., arm numbness, loss of consciousness, partial paralysis, etc.
Causes of a Seizure:
While the exact cause of some seizures can be hard to pinpoint, many seizures can be classified as either provoked or unprovoked. A provoked seizure would include traumatic injuries to the head, whereas an unprovoked seizure would include seizures caused by, for example, a congenital defect.
Unprovoked (“natural”) seizures:
Some seizures may be caused by “natural” phenomena occurring in the body, such as a congenital defect or a chemical imbalance. One example of this is a condition called GLUT-1 deficiency. Other examples include:
genetic factors
congenital (present at birth) problems or conditions
metabolic or chemical imbalances in the body
fever/infection
infection
neurological problems
Alzheimer's disease
unknown reasons
Provoked seizures:
Some seizures are considered provoked if they are caused by an event that happened to the individual. Brain injuries are often the cause of provoked seizures. Other examples include:
birth trauma
alcohol or drugs
head or brain trauma
progressive brain disease
stroke
unknown reasons
brain tumors
Hemimegalencephaly
cortical dysplasia
mesial temporal sclerosis
drug withdrawal
medications
Types of Seizures -
Seizures are divided into two major groups – depending on where they begin in the brain:
Generalized seizures – Unlike partial seizures, generalized seizures seem to begin everywhere in the brain at once. Types of generalized seizures include:
Absence seizures (formerly known as petit mal seizures)
Myoclonic seizures
Clonic seizures
Tonic seizures
Tonic-clonic seizures (formerly known as grand mal seizures)
Atonic seizures (drop attacks)
Partial seizures – Also called “focal” or “local” seizures, partial seizures begin in one location of the brain
Absence Seizures (Petit Mal)
An absence seizure (formerly classified as petit mal), is a very uncommon seizure that begins suddenly and occurs without any warning signs.
People experiencing absence seizures typically appear to stare without moving. Usually lasting less than 15 seconds, absence seizures can occur many times a day and may be mistaken for daydreaming.
While the patient may not remember what happened during the seizure, they’ll typically return to being instantly alert as soon as the seizure is finished.
Treatment of absence (petit mal) seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Myoclonic Seizures
Unlike atonic seizures (which cause the patient’s muscle to go limp), myoclonic seizures (myo meaning “muscle”, clonic meaning “jerk”) result in an increase in muscle tone. The areas of the brain stem responsible for increasing and decreasing muscle tone are close together – meaning atonic and myoclonic seizures probably begin in the same place. Patients experiencing sudden dramatic changes in muscle tone will often suffer from either or both types of seizures.
Patients suffering from myoclonic seizures typically react as if hit by a single jolt of electricity.
Myoclonic seizures are often only one manifestation of a mixed seizure disorder, and they can be very serious. On rare occasions, a patient may suffer from a series of such jolts – a serious type of epilepsy classified as infantile spasms.
It is important to note that not all myoclonic jerks are myoclonic seizures. Think about the times you’ve seen someone falling asleep then suddenly jerk awake. This is a great example of a myoclonic jerk – but not a seizure.|
Treatment of myoclonic seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Tonic and Clonic Seizures
Tonic seizures
During a tonic seizure, the person’s muscles initially stiffen and they lose consciousness. The person’s eyes roll back into their head as the muscles (including those in the chest, arms and legs) contract and the back arches. As the chest muscles tighten, it becomes harder for the person to breathe – the lips and face may take on a bluish hue, and the person may begin to make gargling noises.
Many observers have the misconception that the person is in danger of “swallowing their tongue,” so they attempt to put something in the person’s mouth. Swallowing your tongue is actually impossible, and any attempt to open the now tightly clenched jaw may cause more harm than good.
Clonic seizures
During a clonic seizure, the individual’s muscles begin to spasm and jerk. The elbows, legs and head will flex, and then relax rapidly at first, but the frequency of the spasms will gradually subside until they cease altogether. As the jerking stops, it is common for the person to let out a deep sigh, after which normal breathing resumes.
Tonic-clonic (grand mal) seizures
A tonic seizure is typically accompanied by a clonic seizure – it is rare to experience one without the other. When both are experienced at the same time, this is known as a tonic-clonic seizure (formerly known as a grand mal seizure).
Treatment of tonic and clonic seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Tonic-Clonic (Grand Mal) Seizures
Tonic-clonic seizures (formerly known as grand mal seizures) can be one of the most frightening seizures to observe. There are two parts to a tonic-clonic seizure:
Tonic phase – The person initially stiffens and loses consciousness, causing them to fall to the ground. The person’s eyes roll back into their head as the muscles (including those in the chest, arms and legs) contract and the back arches. As the chest muscles tighten, it becomes harder for the person to breathe – the lips and face may take on a bluish hue, and the person may begin to make gargling noises.
Many observers have the misconception that the person is in danger of “swallowing their tongue,” so they attempt to put something in the person’s mouth. Swallowing your tongue is actually impossible, and any attempt to open the now tightly clenched jaw may cause more harm than good. The tonic phase will typically last no longer than a minute.
Clonic phase – Typically following the tonic phase, the clonic phase will start as the muscles begin to spasm and jerk. The elbows, legs and head will flex then relax rapidly at first, but the frequency of the spasms will gradually subside until they cease altogether. As the jerking stops, it is common for the person to let out a deep sigh, after which normal breathing resumes. The clonic phase will rarely last longer than a few minutes.
As the person transitions from the clonic phase to the post-seizure period, they’ll likely remain unconscious for a few minutes or more, depending on the severity of the seizure. During this time (known as the postictal period), the brain is extremely active trying to stop the cells from firing to bring the seizure under control. When the person wakes up, they may have sore muscles and be tired or confused. The observer’s best course of action is to be assuring and supportive.
Occasionally, it is possible to experience the tonic phase without the clonic phase and vice versa.
Treatment of tonic-clonic (grand mal) seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Atonic Seizures (Drop Attacks)
Unlike myoclonic seizures (which cause muscles to tense), atonic seizures cause the muscles to go limp. The patient’s body may slump or crumple to the ground, possibly causing injury.
The areas of the brain stem responsible for increasing and decreasing muscle tone are close together, which means atonic and myoclonic seizures probably begin in the same place. Patients experiencing sudden dramatic changes in muscle tone will often suffer from either or both types of seizures.
Atonic seizures may be indicative of Lennox-Gastaut Syndrome.
Treatment of atonic seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Partial (Focal) Seizures
Partial (focal) seizures refer to seizures beginning in one area of the brain. By observing which area of the body is affected by the seizure, physicians can identify where in the brain the seizure occurred.
Partial seizures are further categorized as either:
Simple partial seizures – The seizure is localized to one area on one side of the brain, but may spread to other areas. Consciousness is not lost during a simple partial seizure.
Complex partial seizures – Seizures originating in one area of the brain that affect consciousness are labeled as complex partial seizures.
Partial seizures that secondarily generalize – Partial seizures may spread to other areas of the brain.
Complex Partial Seizures
Complex partial seizures can begin in any lobe of the brain, but cause alteration of awareness due to spreading of seizure activity.
Complex partial seizures are often preceded by a simple partial seizure (aura). An aura is often described as a warning and can manifest in several different ways, such as a sense of fear, a funny feeling in the body, déjà vu, etc.
Patients experiencing a complex partial seizure may stare blankly into space, or experience automatisms (non-purposeful, repetitive movements).
Treatment of complex partial seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Simple Partial Seizures
Simple partial seizures are localized to one area on one side of the brain, but may spread from there. Consciousness is not lost during a simple partial seizure. The left side of the brain controls the right side of the body, and the right side of the brain controls the left side – so it can be relatively easy for a doctor to identify which side of the brain is being affected by a simple partial seizure.
Physicians typically break simple partial seizures down into four areas, depending on the location in the brain and parts of the body affected:
Motor – A simple partial seizure with motor symptoms will affect muscle activity, causing jerking movements of the foot, face, arm, or another part of the body. Physicians can diagnose which side of the brain is affected by observing which side of the body experiences symptoms (left brain controls right side, right brain controls left side).
Sensory – A simple partial seizure with sensory symptoms affect the senses: hearing problems, possible hallucinations, and other distortions.
Autonomic – A simple partial seizure with autonomic symptoms affects the part of the brain responsible for involuntary functions: it may cause changes in blood pressure, heart rhythm, bowel function, etc.
Psychic – A simple partial seizure with psychic symptoms affects parts of the brain that trigger emotions or previous experiences: it may cause feelings of fear, anxiety, déjà vu (the feeling that something has been experienced before), etc.
Treatment of simple partial seizures
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Partial Seizures that Secondarily Generalize
Partial (focal) seizures refer to seizures occurring in one or more areas on one side of the brain – in other words, they begin in a limited area of the brain. Instead of remaining in the original area, the seizure may spread to other areas of the brain, thus affecting other areas of the body.
When a partial seizure spreads to the other side of the brain, it is known to “secondarily generalize.” Partial seizures that secondarily generalize may include convulsions or spasms, a loss of muscle tone, or a decrease in muscle tone.
Treatment of partial seizures that secondarily generalize
There is no one treatment method for any patient with a seizure disorder. Each treatment plan is tailored to the individual patient based on their diagnosis and symptoms. Treatment options may include medical therapy, nerve stimulation, dietary therapy, or surgery, as appropriate. Clinical trials may also be a valuable treatment alternative.
Learn more here.
I am one of the million out of 3million living in America that cannot get well by any medication due to Epilepsy. There is more death caused by Epilepsy around the world and there are 65 million people worldwide that suffer. Each year over 150,000 people are newly diagnosed with Epilepsy. 30% of them are children. Not only that but epileptics have a 3-6 times greater risk of premature death. In America, Epilepsy is twice as common as breast cancer and takes as many lives, but you will never hear or see anybody putting their foot down about it and I intend to change that. Approximately 1 in 26 people in the United States will develop Epilepsy at some point in their lifetime. Learn more here.
Electroencephalography (EEG)’s, Magnetic Resonance Imaging (MRI)’s and Ambulatory Electroencephalography (AEEG)’s are not fun, but necessary:
And EEG consists of 24 electrodes/wires plastered on one's head with a special medical needle and glue. This is commonly an outpatient procedure, but many epileptics may be in for a number of days. In my experience, I have been pinched with a needle on my scalp five or more times per day by different nurses when one of the electrodes became loose. On the chest, 2 electrodes are placed, one on the right and one on the left. At the end of this procedure which can last from one hour to up to two weeks, pulling the electrodes off is quite painful, but means you are happily going home. I have however yanked the electrodes off my head during seizures at the hospital which has led to the processbeing redone. It’s a cruel joke when you look down and you have 26 wires in your hand. Every time I go to have an EEG done, I ask the nurse, “When are the electrodes going to just be placed into the cloth on my head instead of being glued onto my scalp?" The answer is that they used to do it that way in the past, but the results were not as accurate. Possibly, they will do this again in the future.
An AEEG is similar but different in that it’s a couple of days that your neurologist wishes to see data, so you have a recording device at you side, all the same electrodes and a white cloth on your head. When I was working full time, I asked my boss if it would be ok to come in with a baseball cap on to cover the wires. He hates caps at work, but made an exception for me. The only problem was that working behind a computer at the time, did not show any results. It was different then today when I can trigger a seizure just by closing my eyes.
An MRI is a much more simple, painless study of one lying on a bed with a cushion and half of your body going into a tunnel for about 20 to 30 minutes. As a child, they would offer you music to listen to. If a seizure occurs, you will awaken a slam your head from side to side against the machine. Luckily this has never happened to me, I usually fall asleep plus I’d rather have an MRI done then an EEG, but the results from an EEG are more accurate, unfortunately.
Source: VNS Stimulator
In February 2009 I implanted a device in me that seemed promising at the time. The Vagus Nerve Stimulator, the (VNS). The operation was a simple outpatient procedure where they implant a small device behind the left pectoral muscle the size of a hearing aid that has an irremovable metal piece attached to the vagus nerve in your throat. It is supposed to send signals to your brain from the nerve. The video I received showed a lot of hope, but you can really be successful if you are part of the 1% that this works for 100% in controlling seizures, then you are a very lucky person. Otherwise like most, you will have it implanted into you and not sure if it is working correctly or not. Your neurologist will ask you how you feel - better, worse or the same. I myself am not sure if it is or isn’t working for the better but I can tell you this, it isn’t a total cure for me at least. The VNS is controlled by your neurologist and can be changed to a few different settings from rapid, setting it off 7 seconds a minute which I’ve had done to 30 seconds every 3 minutes or 30 seconds for every 5 minutes. The neurologist programs the strength and timing of the impulses according to each patient's needs. The settings can be programmed and changed by placing a wand over the generator on the left side of the chest. The wand is connected to a handheld computer. The stimulator does come with its own magnetic devise that you keep in your pocket which can activate it simply by placing it over your pectoral muscle sending a quite painful burning sensation to your throat for 30 seconds when and if you can sense an episode occurring. I used to do this when I was a younger man, as I did get auras - which is when you feel a seizure is about to occur about 10 seconds prior and are able to stop it from happening. This had been gone already when I had the VNS installed. I did carry the magnet with me in the past to work but was never able to use it for anything good and promising. The VNS magnet has also one other purpose, to hold it over the device for a minute to shut it down, but I would not recommend it without orders from your neurologist. It is not a dangerous devise and no side-affects have occurred other than my throat tightening up every 3 minutes for 30 seconds making it very difficult for anyone to understand what I am saying, on the phone or in person. The phone being the worst of it because people tend to hang up on important phone calls because they think that you’ve gone or done something wrong when all you wanted to do was speak to them. Some of my friends who remember me or my family know that my voice it pretty hoarse already so my throat becoming even more hoarse makes it difficult to hold conversations.
I tried having brain surgery, but my doctors found out at NYUMC that my Temporal Lobe Epilepsy was not just on the right side of my brain, but also the left. The Temporal Lobe is a part of the brain where humans complete all their main functions. This also affects memory, which is why most epileptics have memory loss. It was said to me by a neurologist, that if my epilepsy existed in the frontal region than surgery would be possible without any severe side-affects. Since mine exists on the back of the brain, cutting it out would be a dangerous idea, therefore the surgery was too risky to perform. No surgeon in America will take the chance. If it had been on one side, the surgery would have given me 100% definite loss of my peripheral vision which in turn is tunnel vision the rest of my life. Possibly even TOTAL blindness. The best thing that I have going for me is my vision, which it is not affected by my seizures. Even if the surgery had been a success, I would still have to be on medication for the rest of my life and the tunnel vision would have caused a definite inability of ever driving again, which is no concern to me anymore. The way you see people drive on the road would just be a cause for disaster.
THE KETOGENIC DIET
The Ketogenic Diet, 100% sugar free and low carb diet. This is not a diet that was so necessary for me but my neurologist for some reason had a problem with my weight because I was forty pounds heavier than back during my working days. I had tried the diet a year before but not to the full extent, but now my dietician thought that it would help so I went through with it with Michelle’s help. Cooking with the right oils - coconut, as well as getting me the right breads with fibers. It is a high fat, no sugar, low carb and high protein diet.
Nutricia Ketocal on the other hand, sold as a liquid or ppo po powder, is frequently used to treat Epilepsy that's high in fat and low in carbohydrates. The special diet forces the body to make extra ketones, natural chemicals that suppress seizures. It's mainly recommended for epileptic patients who don't respond to treatment.
This test is done morning or night by a urine stick to test the strength or level of your ketones from pale to strong but hasn’t worked well for me. I had started the diet in the hospital as usual under the watch of the nurses and the EEG monitoring me. The first and second days the neurologist there had me drink five shakes. The third day I drank two - so I would imagine drinking twelve shakes in three days had shown much better results. A few days later back at home I was to take one a day as informed, but it didn’t seem to be at all helping.
I will stay on this diet because I like it but will drop the ketocal from it. This diet I was told works better on children then adults because most adults cannot stick to the strict diet as easy as a child. Gluten free pizza and such may work for a diabetic, but still have the same carb intake of a regular pizza. Not to mention that being Italian and dropping every piece of bread and pasta from my daily life is hard. I found ways to work around it without suffering the consequences.
HEMP OIL
Another thing I use that tastes good is Hemp Oil. Hemp oil has nature's ideal 3:1 Omega-6 to Omega-3 ratio. Unlike flax, hemp has valuable Super Omega-3 (SDA) and Super Omega-6 (GLA) which can help the body metabolize fat. This one in particular made by Nutiva is to enjoy our delicious, unrefined, cold pressed, certified-organic Canadian hemp oil, hemp has Omega-3, the good fat" doctors recommend for optimal health.
It’s an oil that has been around and used by epileptics for hundreds of years. This oil is actually made from raw organic hempseed oil. This oil must be kept cold wherever you buy it from and refrigerated and never to be used to fry with. It can be used on top of anything you wish to eat after it is cooked - meats, fishes, pasta dishes, dinner salads, or even smoothies or breakfast eggs. Once you get used to using it, it doesn’t taste bad at all. The only thing strange about it is that it’s green so if you do use it on an omelet, you’ll be eating your green eggs.
Take a table spoon, open the cold jar up, poor it on the spoon and onto whatever food you wish. If you’re wondering if it helps, I believe so. My wife and I did not hear about this from my neurologist or dietitian but on our own research. He and she knew about it of course when we told them that I was using it and they had no complaints towards it. You will find that this Hemp Extract such as the one used for Charlotte’s Web and many adult marijuana supplements works wonders.